Vitamin D Supplements: A Double-Edged Sword for Health Risks
Written on
Understanding the Dual Nature of Vitamin D Supplementation
Recent randomized trials have revealed that Vitamin D supplementation could potentially lower cancer risk while simultaneously increasing the risk of heart disease.
Imagine a grand cathedral dedicated to the principle that correlation does not imply causation. Walking through its ornate doors, you might view various associations, such as the curious link between ice cream sales and shark attacks, or the positive effects of red wine on heart health. Upon reaching the altar, you find the emblematic figure of Vitamin D, a supplement widely revered but often misunderstood.
If you've followed the discourse around this supplement, you know there's considerable skepticism regarding its efficacy. In clinical research, no other compound showcases such strong correlations with health outcomes while simultaneously lacking robust evidence for causation.
Low levels of serum Vitamin D have been associated with increased risks of various ailments, including heart disease, cancer, and even infections like COVID-19 and C. diff. However, randomized controlled trials (RCTs) that aim to establish causal relationships often yield disappointing results.
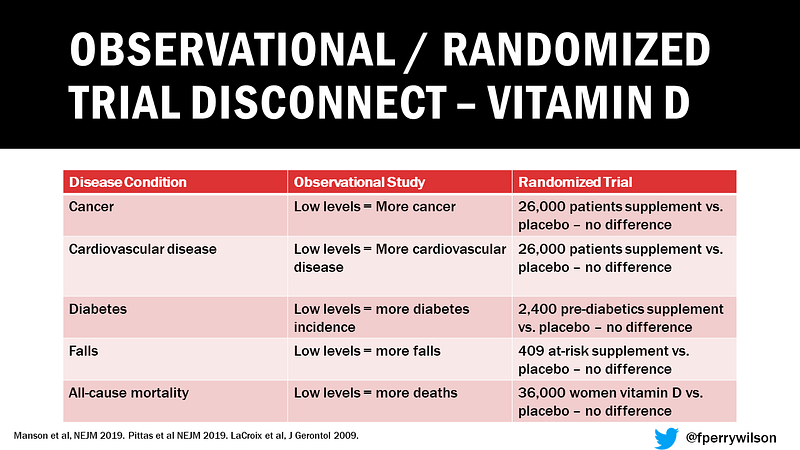
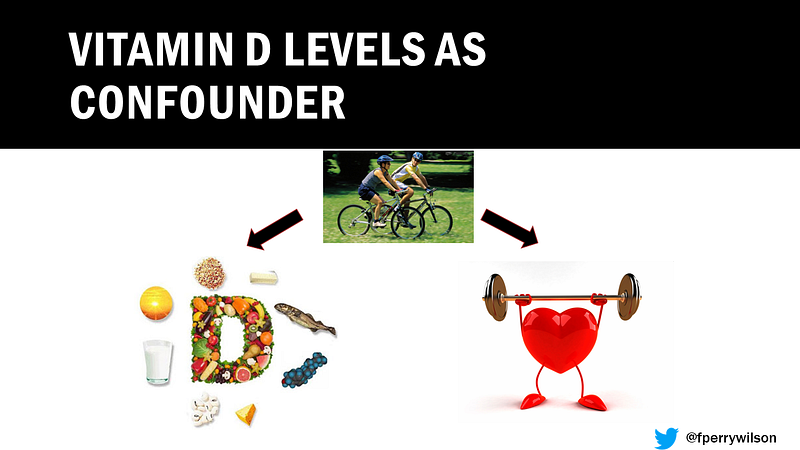
While RCTs are not without flaws, they prompt us to either defend Vitamin D vehemently—suggesting we ignore the findings of these trials and invest in this $800 million industry—or to recognize that Vitamin D levels might merely reflect various lifestyle factors associated with better health outcomes, such as exercise and a balanced diet.
Alternatively, it is conceivable that Vitamin D supplements do exert some influence, albeit counterbalanced by detrimental effects. Stay tuned for more insights.
The Women's Health Initiative (WHI) is one of the most significant studies examining the effects of Vitamin D and calcium supplementation. This trial has been a major contributor to the prevailing negative outcomes associated with Vitamin D supplementation.
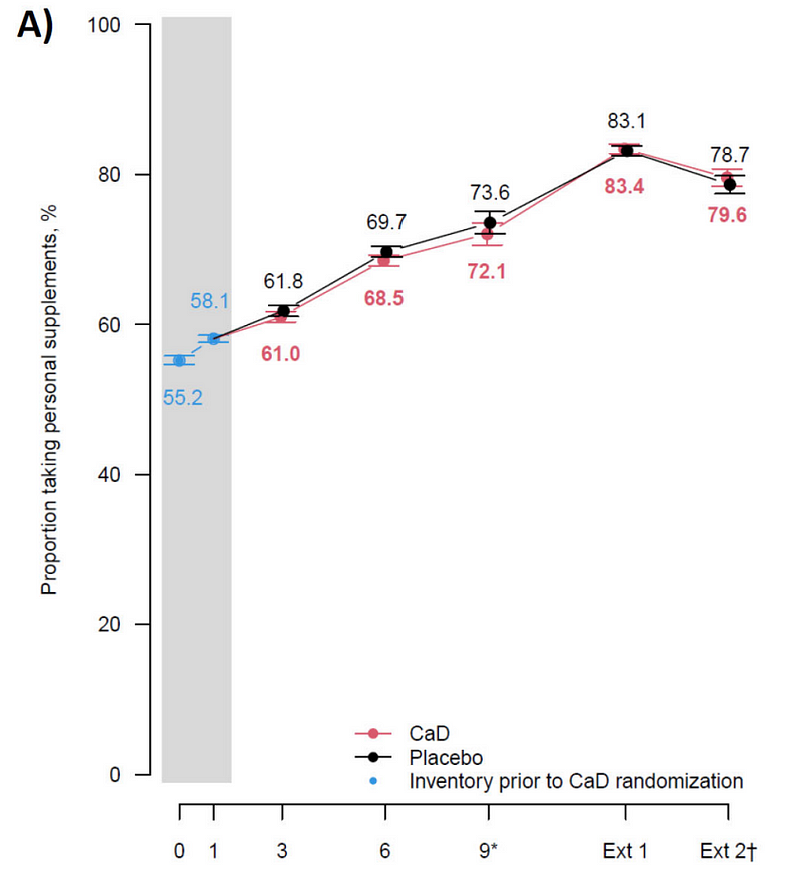
However, a closer examination of the WHI's inclusion and exclusion criteria reveals that participants were permitted to continue taking vitamins and supplements, irrespective of their randomization status. Consequently, many individuals entered the trial already using supplements, which could skew the results.
According to the original analysis, randomization to Vitamin D supplementation did not show any significant effects on cancer or cardiovascular outcomes. Yet, with three decades of follow-up, a recent study published in the Annals of Internal Medicine revisits these findings.
Led by Dr. Cynthia Thompson from the University of Arizona, this updated analysis examines two crucial yet previously unconfirmed outcomes: the potential reduction in cancer risk and the possible increase in heart disease risk from Vitamin D supplementation.
The initial randomized trial lasted seven years, but the analysis now encompasses outcomes observed over a span of approximately 20 years. The researchers argue that since cancer and heart disease take time to manifest, historical Vitamin D supplementation might either provide benefits or pose risks.
Now, let’s delve into the findings. Participants assigned to Vitamin D and calcium supplements saw a 7% decrease in cancer mortality, particularly from colorectal cancer, which was statistically significant. Conversely, there was a 6% increase in cardiovascular disease mortality among those receiving supplementation, leading to no overall change in all-cause mortality rates.
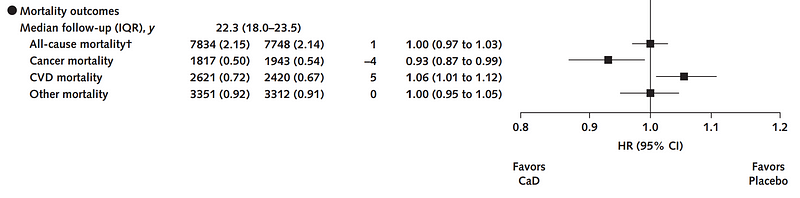
You might wonder about the implications of external supplementation on these results. The researchers clarify that those supplementing outside the trial had higher baseline Vitamin D levels, which could indicate healthier lifestyle choices, further complicating the analysis.
To isolate the effects of randomization, the authors focused on participants who did not take external supplements. Among this group, there was an 11% reduction in cancer incidence—statistically significant—but the effect on cancer mortality did not reach significance. Importantly, there was no corresponding increase in cardiovascular disease.
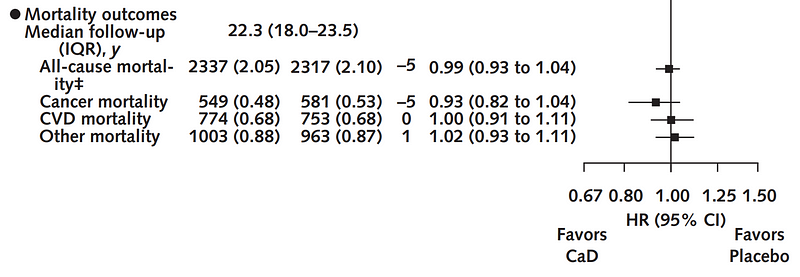
It's worth noting that many participants entered the trial with Vitamin D levels below the established deficiency threshold. However, a lack of stratified data based on baseline Vitamin D levels hinders a clear understanding of these outcomes.
Ultimately, it appears that for most women, Vitamin D supplementation may not significantly impact mortality rates. While it might slightly decrease the risk of certain cancers, it could also elevate the risk of heart disease. Personalized approaches may be beneficial, particularly for those with a family history of cancer or heart disease risk factors. This strategy warrants further exploration through clinical trials, ideally ensuring that participants refrain from additional supplement use.
A version of this commentary first appeared on Medscape.com.
Chapter 2: Exploring Vitamin D's Complex Relationship with Health
This video titled "Vitamin D Supplements May Be a Double Edged Sword" delves into the contradictory evidence surrounding Vitamin D supplementation, highlighting both potential benefits and risks.
In this video, "Coronavirus and Vitamin D: Correlation, Causation, and Confusion," experts discuss the complexities of Vitamin D's role in immunity and health outcomes during the pandemic.